On Target: Helpful Blood Glucose Goals For People With Prediabetes
It is time to understand your blood glucose results for monitoring and using a continuous glucose monitor.
Sandy was recently told she has prediabetes. Her first question was, “What are my numbers supposed to be?” This article explores the target blood sugar and how to understand your results for monitoring and using a continuous glucose monitor.
It is difficult to sort out the many numbers associated with prediabetes and diabetes, especially if you are newly diagnosed. Sandy was told she had prediabetes because her A1C was at 5.8. The A1C test is a 3-month average of your blood glucose. It can be used to diagnose prediabetes and diabetes. Learn how prediabetes and diabetes are diagnosed.
The No Weight Loss Required newsletter provides helpful information on using a non-dieting, weight-inclusive approach to managing blood sugars. A long time ago, I understood that dieting didn’t work and you can’t hate yourself well. I have taken this effort in several directions, including writing five books and starting a non-profit (The Center for Mindful Eating).
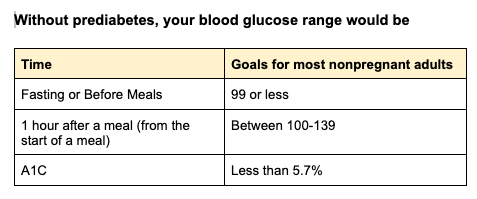
However, the individual number used to be diagnosed with prediabetes or diabetes is not the blood glucose range used as your glucose goal. The three charts list the blood glucose targets for someone without diabetes, someone with prediabetes, and someone with diabetes. This information can help you after you have been diagnosed with prediabetes or diabetes.
What does it mean if my blood glucose is higher or lower than these numbers?
Individual blood glucose readings can make you curious, but they can’t tell the whole story. Blood glucose readings fluctuate, meaning they change for many reasons. Some are related to food and exercise, and some are not. As noted above, these are blood glucose targets, and when taken together, they can give you an understanding of your blood glucose range.
How frequently do I check my blood sugar?
That is a great question, and it depends on some other factors.
Is this a new diagnosis?
Has there been a recent change in your health?
Are you on a new medication that impacts blood glucose?
Are you having symptoms of high or low blood glucose?
If you answered yes to these questions, checking more often can help you understand what is happening. It can also help your provider adjust your medication and connect your experience with your blood glucose.
Checking in the morning when you wake up is helpful. It can help you and your provider evaluate your fasting blood glucose, which because you were sleeping, is a time when you can’t eat less or exercise more!
Checking after eating (1-2 hours after the start of a meal) helps understand how some meals impact blood glucose. For example, you may learn that cereal impacts blood glucose differently than broccoli or eggs.
Checking after exercise can help you learn how activity impacts blood glucose.
Checking before and after a meal can help you understand how much your blood glucose rises. For example, if Sandy didn’t know her blood glucose level before eating, she could only learn if it was within the range after eating. It is helpful information but doesn’t tell the whole story. For example, if Sandy’s blood glucose level was 220 mg/dL before a meal and went to 240 mg/dL after eating, it rose 20 points, which isn’t very much. However, if she only checked after eating, she might assume that the elevated blood glucose reading was because of something eaten, which wasn’t the case. (Remember, Sandy’s glucose only rose 20 points from eating.)
Checking when you feel funny—headache, dizzy, confused, hungry, or irritable—can help you understand if these symptoms are related to your blood sugar or if you are having a terrible day!
Checking at bedtime can help you see if your blood glucose changes when you sleep.
Stay curious!
Ask, “Why is my blood sugar low or elevated? Become a detective and try to explain (without always blaming your diet) what could explain this result. Look for patterns in your blood sugar. Most meters have phone apps that make it easier to see patterns. Here is a list of trusted apps: https://diabetesed.net/apps-for-diabetes/. Make notes when you understand your blood sugar. I strongly suggest you write these on paper or in your blood sugar tracking app. It will help you remember to ask questions when it isn't making sense at your next diabetes appointment.
What about Using A Continuous Glucose Monitor?
The Continuous Glucose Monitor System, CGMS, is a device worn that measures the glucose in the fluid surrounding your cells. The blood glucose targets are the same, but because the sensor checks more frequently, it can help you spot trends.
I have prediabetes, and I am sharing my CGMS report to explain what you might see. I am using a Libre 2 sensor. The first report is called the Ambulatory Glucose Profile, AGP report.
Points to notice:
How long was the sensor worn? It was worn for 14 days, and this sensor captured about 94% of the data.
The average glucose is 105. This number averages all the blood glucose readings. This can decrease this number if your sensor records several low blood glucose readings (as my report did). Looking at the blood glucose in isolation doesn’t provide insight into glucose patterns or highlight opportunities.
Dexcom, a CGMS manufacturer, explains that the Glucose Management Indicator “approximates the laboratory A1C level expected based on average glucose measured using continuous glucose monitoring (CGM) values. Average glucose is derived from at least 12 days of CGM data.”
Time in Range: This is the CGM metric most commonly used to guide diabetes management. Five CGM-defined categories create the target range graph above.
Next is a screenshot of blood sugars. Sensors take time to calibrate and may be inaccurate for the first 24 hours. Additionally, when blood glucose changes, the sensor's accuracy is less.
In the image above, you can see a gray band. It represents the target range of 70-180 mg/dL. Numbers that are above or below the target range change color. This image shows my blood sugars dipping low around 9 - 11 pm. You can also see that at 9 pm, I checked my blood glucose with my meter. The sensor said my blood glucose was 89, but the meter said it was 108. It suggests that the 63 and 53 readings were more likely 83 and 73, not low blood glucose. Check-in and see if you have any physical symptoms of low blood sugar.
TIP
Use a meter to check the accuracy of your sensor. The low blood sugars recorded on my CGMS are likely due to changing blood sugar. I suspect this because I do not take any medications that would cause a hypoglycemic reaction.
As previously suggested, mark meals and exercise. It helps you identify possible ways to adjust your lifestyle, activity, or diet. You can see where notes were taken, including when I woke up, at, or had a low blood glucose reading.
If possible, record and estimate the carbohydrates you ate.
Individual Sessions: I offer virtual appointments for clients via Nourish. I am currently licensed in the following states: AK, AZ, CA, CO, CT, FL, GA, HI, ID, IN, MA, MI, NH, NJ, NY, OK, OR, PA, TX, UT, VA, VT, WA, WI, WV, and WY.